Science offers the boldest metaphysics of the age. It is a thoroughly human construct, driven by the faith that if we dream, press to discover, explain, and dream again, thereby plunging repeatedly into new terrain, the world will somehow come clearer and we will grasp the true strangeness of the universe. And the strangeness will all prove to be connected and make sense.
~ Edward O Wilson ~
Consilience: The Unity of Knowledge
~ Edward O Wilson ~
Consilience: The Unity of Knowledge
I arrived with considerable trepidation, to this place I adamantly opposed. To think for even a moment, that a deeply dissociative population of traumatized and dangerously depressed individuals would benefit from a treatment that itself elicits a dissociative state, was not just absurd on the face of it, but downright antithetical to what I knew to be true about a traumatized brain, on every level from the psychological to the cellular. And yet, an ever-growing body of scientific data concerning off-label use of ketamine with the deeply dissociative populations I have been treating for forty years, was proving otherwise.
Anecdotal accounts of relief from bone-crushing intractable major depression in under two hours, immediate cessation of dangerous, psychically wounding suicidal ideation, an amazing respite from gruesome combat-related flashbacks, or the otherwise unrelenting technicolor images of equally gruesome childhood abuse; all from a surgical anesthetic that has been around for more than 60-years with excellent pharmacovigilance (the larger underground market all-too familiar with special-k notwithstanding), was certainly worth a deep-dive.
The unmitigated speed with which ketamine divined its magic, conjured initial images of Barbara Eden folding her arms and bowing her head in a trigeminal-mediated head toss, were soon replaced with a milder skepticism if not of hope, but rather, the secret wish of 'what if'.
The Ketamine - Depression Connection
Developed in the 1950s, phencyclidine (PCP) better known as angel dust, was a widely used intravenous anesthetic until its demise not a moment too soon, directly attributable to a maelstrom of dangerous and occasional fatal side-effects that included vivid long-lasting hallucinations and psychosis. The rush was on to find a replacement. In 1962, American chemist Calvin L. Stevens, while employed at Parke-Davis, was the first to synthesize ketamine. Within a year of discovery, ketamine replaced PCP and was patented for use in human sedation, as clinical trials to evaluate for safety and efficacy were underway. In 1970, Ketamine received FDA approval as an anesthetic for human and veterinary use.
A dearth of medical data by a cadre of post op patients professed their ketamine experience as variations on the theme of 'pleasant', 'dreamy' and 'heavenly', referring to ketamine's dissociative quality. As more and more data began rapidly accumulating, given what we knew to be true with PCP, the data was taken in stride. Until something else entirely, emerged from medical files from distant locations. Multitudinous accounts of patients with treatment-resistant depression, a disorder not necessarily known to their respective treatment teams, claiming that immediately following their procedure, they suddenly found themselves in remission from depressive symptoms. Not only was this a serendipitous find, but it rocked the foundation of what we knew to be true concerning the neural underpinnings of depression and antidepressant medication.
The 1960s ushered in a new wave of interest in depression, challenging the wider mechanisms involved, and the specificity of antidepressants on targeted neurotransmitters. With it, came the advent of a newer line of antidepressant medications including Fluoxetine, the first selective-serotonin-reuptake-inhibiters (SSRIs) commercially available as Prozac. The year was 1989, but the well-regarded monoamine hypothesis of depression was a product of the 50s and it was high time for a revamp. During the first several years of SSRI history, the tricyclic antidepressants were still available. Despite the fact that both SSRIs and tricyclics impact serotonin, the tricyclics came with a veritable laundry list of side-effects ranging from the annoying to the dangerous and as such they were already being phased out. What was new and important news however, was the realization that the two known classes of antidepressants, both relieved symptoms of depression by increasing levels of monoamine neurotransmitters, falsely confirming that in fact, depression was caused by a deficiency in these specific neurotransmitters. Ketamine was soon to open Pandora's box; if ketamine acted on the glutamatergic system, and does not target the monoamines, how then, did a single administration of intravenous ketamine, whose primary mechanism of action does not involve the monoamine neurotransmitters of serotonin, dopamine, and norepinephrine, cause an immediate cessation and dramatic remission of depressive symptoms?
What is Ketamine
Classified as a hallucinogen, ketamine is referred to as a dissociative anesthetic chemically known as (RS)-2-(2-chlorophenyl)-2-(methylamino)-cyclohexanone.
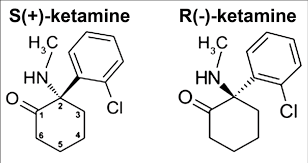
Ketamine is a chiral compound, in that it exists in two enantiomeric forms. Enantiomers are mirror-image isomers of a compound that cannot be superimposed onto each other (hence, mirror image). While enantiomers have the same molecular formula, they have different structural arrangements. As such, different enantiomers produce a different biological effect. Ketamine has two enantiomers referred to as S-(+) ketamine or esketamine, and R-(-) ketamine or arketamine. The nasal spray Spravato uses esketamine only. Ketalar, Ketanest, and Ketaset each use a 50/50 racemic mixture of ketamine dissolved in saline, that includes both esketamine are arketamine.
S-ketamine has traditionally been shown to be the more potent enantiomer and is responsible for most of ketamine's anesthetic and analgesic effects. It has a higher affinity for NMDA receptors (discussed in the following section), which is believed to be a key mechanism of ketamine's action. R-ketamine, on the other hand, has weaker NMDA receptor activity and is less potent overall. Notwithstanding, it is thought to have some unique properties and may contribute to ketamine's antidepressant effects. It has been suggested that R-ketamine may interact with receptors other than NMDA, such as the opioid and sigma receptors, which might play a role in its antidepressant activity.
In addition to the FDA-approved Spravato for TRD, Ketamine is sold under the Ketalar, Ketanest, and Ketaset name brands for use in IV and IM administration as an anesthetic and an analgesic and for off-label use.
Anecdotal accounts of relief from bone-crushing intractable major depression in under two hours, immediate cessation of dangerous, psychically wounding suicidal ideation, an amazing respite from gruesome combat-related flashbacks, or the otherwise unrelenting technicolor images of equally gruesome childhood abuse; all from a surgical anesthetic that has been around for more than 60-years with excellent pharmacovigilance (the larger underground market all-too familiar with special-k notwithstanding), was certainly worth a deep-dive.
The unmitigated speed with which ketamine divined its magic, conjured initial images of Barbara Eden folding her arms and bowing her head in a trigeminal-mediated head toss, were soon replaced with a milder skepticism if not of hope, but rather, the secret wish of 'what if'.
The Ketamine - Depression Connection
Developed in the 1950s, phencyclidine (PCP) better known as angel dust, was a widely used intravenous anesthetic until its demise not a moment too soon, directly attributable to a maelstrom of dangerous and occasional fatal side-effects that included vivid long-lasting hallucinations and psychosis. The rush was on to find a replacement. In 1962, American chemist Calvin L. Stevens, while employed at Parke-Davis, was the first to synthesize ketamine. Within a year of discovery, ketamine replaced PCP and was patented for use in human sedation, as clinical trials to evaluate for safety and efficacy were underway. In 1970, Ketamine received FDA approval as an anesthetic for human and veterinary use.
A dearth of medical data by a cadre of post op patients professed their ketamine experience as variations on the theme of 'pleasant', 'dreamy' and 'heavenly', referring to ketamine's dissociative quality. As more and more data began rapidly accumulating, given what we knew to be true with PCP, the data was taken in stride. Until something else entirely, emerged from medical files from distant locations. Multitudinous accounts of patients with treatment-resistant depression, a disorder not necessarily known to their respective treatment teams, claiming that immediately following their procedure, they suddenly found themselves in remission from depressive symptoms. Not only was this a serendipitous find, but it rocked the foundation of what we knew to be true concerning the neural underpinnings of depression and antidepressant medication.
The 1960s ushered in a new wave of interest in depression, challenging the wider mechanisms involved, and the specificity of antidepressants on targeted neurotransmitters. With it, came the advent of a newer line of antidepressant medications including Fluoxetine, the first selective-serotonin-reuptake-inhibiters (SSRIs) commercially available as Prozac. The year was 1989, but the well-regarded monoamine hypothesis of depression was a product of the 50s and it was high time for a revamp. During the first several years of SSRI history, the tricyclic antidepressants were still available. Despite the fact that both SSRIs and tricyclics impact serotonin, the tricyclics came with a veritable laundry list of side-effects ranging from the annoying to the dangerous and as such they were already being phased out. What was new and important news however, was the realization that the two known classes of antidepressants, both relieved symptoms of depression by increasing levels of monoamine neurotransmitters, falsely confirming that in fact, depression was caused by a deficiency in these specific neurotransmitters. Ketamine was soon to open Pandora's box; if ketamine acted on the glutamatergic system, and does not target the monoamines, how then, did a single administration of intravenous ketamine, whose primary mechanism of action does not involve the monoamine neurotransmitters of serotonin, dopamine, and norepinephrine, cause an immediate cessation and dramatic remission of depressive symptoms?
What is Ketamine
Classified as a hallucinogen, ketamine is referred to as a dissociative anesthetic chemically known as (RS)-2-(2-chlorophenyl)-2-(methylamino)-cyclohexanone.
Ketamine is a chiral compound, in that it exists in two enantiomeric forms. Enantiomers are mirror-image isomers of a compound that cannot be superimposed onto each other (hence, mirror image). While enantiomers have the same molecular formula, they have different structural arrangements. As such, different enantiomers produce a different biological effect. Ketamine has two enantiomers referred to as S-(+) ketamine or esketamine, and R-(-) ketamine or arketamine. The nasal spray Spravato uses esketamine only. Ketalar, Ketanest, and Ketaset each use a 50/50 racemic mixture of ketamine dissolved in saline, that includes both esketamine are arketamine.
S-ketamine has traditionally been shown to be the more potent enantiomer and is responsible for most of ketamine's anesthetic and analgesic effects. It has a higher affinity for NMDA receptors (discussed in the following section), which is believed to be a key mechanism of ketamine's action. R-ketamine, on the other hand, has weaker NMDA receptor activity and is less potent overall. Notwithstanding, it is thought to have some unique properties and may contribute to ketamine's antidepressant effects. It has been suggested that R-ketamine may interact with receptors other than NMDA, such as the opioid and sigma receptors, which might play a role in its antidepressant activity.
In addition to the FDA-approved Spravato for TRD, Ketamine is sold under the Ketalar, Ketanest, and Ketaset name brands for use in IV and IM administration as an anesthetic and an analgesic and for off-label use.
Mechanism of Action
Ketamine is classified as an NMDA receptor antagonist meaning, it blocks the activity of N-methyl-D-aspartate (NMDA), which is involved in the transmission of pain signals, learning, memory, and mood regulation. Although the exact mechanism of action for ketamine is not fully understood, it does involve interactions with an array of different neurotransmitter systems, most notably glutamate, the primary excitatory neurotransmitter in the brain. Its effects are modulated by the NMDA receptors. When ketamine blocks NMDA receptors, glutamatergic signaling is disrupted.
When NMDA receptors are blocked, it triggers a compensatory increase in the release of glutamate, leading to an overall increase in glutamate activity including gamma-amniobutyric acid (GABA), dopamine, and serotonin. This modulation of neurotransmitters is thought to contribute to ketamine's effect of pain perception, mood, and cognition. Ketamine also interacts with opioid receptors which may further contribute to its analgesic and antidepressant effects. Of particular interest, ketamine has been found to increase the release of brain-derived neurotrophic factor (BDNF), a protein that supports the survival of existing neurons, the growth and differentiation of new neurons and synapses, and the ability for synapses to change and adapt over time, the process known as synaptic plasticity.
BDNF has its greatest effect on the hippocampus, an areas of the limbic system responsible for memory and learning. BDNF is a vital for long-term potentiation (LTP), a process that increases synaptic strength as well as a key mechanism for learning and memory. Disruption to the hippocampus is directly implicated in Alzheimer's disease, epilepsy, depression, post-traumatic stress disorder (PTSD), and the consolidation of memory from short- to long term memory, typical of the selective memory of trauma survivors..
There is also a wealth of evidence that ketamine elicits an effect on alpha-amino hydroxy methyl isoxazole propionic acid (AMPA), an important pathway for the regulation of mood, a significant factor in the rapid relief of depressive symptomotology.
Off-Label And Current Uses
The National Institute of Mental Health (NIMH) developed the protocol for ketamine infusion therapy for off-label psychiatric use as 0.5 mg/kg to 1.0 mg/kg of racemic ketamine infused in saline for a 40-minute duration. Interestingly, studies found evidence that the preferential dose for an opioid population is a slightly higher initial dose at 0.75 mg/kg per dose.
A flood of research over the past few years concerning the use of off-label ketamine has demonstrated that both intravenous (IV) and intramuscular (IM) administration of subanesthetic doses are providing a robust, rapid, and transient antidepressive and anti-suicidal effect for TRD with suicidality, with no differentiation of effect between the two modes of administration. As it awaits FDA approval, ketamine is legally approved for off-label use in treating PTSD and C-PTSD, OCD, alcohol and opioid addiction, generalized anxiety disorder (GAD), unipolar depression and bipolar disorder, and anorexia.
A recent addition to the ketamine armamentaria is the use of sublingual ketamine lozenges for at-home use supplied through ketamine-approved providers. Although current research shows a slightly superior bioavailability and control of dosage with IV administration, efficacy rates for IV, IM, oral sublingual, and nasal administration are found to be undifferentiated, with intranasal administration requiring a 10-pump single-action dose for the same effect.
On March 5th, 2019, the FDA approved ketamine as an intranasal spray branded by Janssen's Neuroscience division, as Spravato, who, in effect won the lottery, and was granted use under a Risk Evaluation and Mitigation Strategy (REMS), TRD. To date, Spravato remains a Schedule III controlled substance, self-administered on site and monitored by a ketamine-certified physician, expressly for TRD with high risk of suicide.
Research has also demonstrated that ketamine is showing success for PTSD and C-PTSD, Obsessive-Compulsive Disorder (OCD), Addiction, especially for opioid addiction, and Generalized Anxiety Disorder (GAD). It should be stated at this point that off-label use of ketamine is only available for adults. Recent studies have shown similar success with OCD when adding Lamotrigine. There is not enough data to determine the effects of ketamine on the adolescent brain.
Whether FDA-approved Spravato or off-label usage, ketamine is not a first-line treatment, and at least for now, providers are prohibited from offering the treatment to anyone without a clinician referral. In the same way that antidepressant and mood stabilizing medications are never meant for use in place of psychotherapy, the protocol for the use of any legitimate ketamine treatment in a psychiatric population requires adjuvant cognitive-behavioral therapy (CBT), preferably during, and after a ketamine treatment.
Ketamine Treatment vs Ketamine-Assisted-Psychotherapy (KAP)
While the standard protocol for ketamine administration in a psychiatric population specifies the concomitant use of CBT, there is distinct difference in the sequencing of events between Ketamine treatment and KAP replete with a fair amount of controversy over best practices. This appears to have caused some confusion. Hoping to clear the confusion, the two methods are described below...
Ketamine treatment simply refers to receiving the drug from a ketamine-certified provider, who is a physician or psychiatrist (or a nurse practitioner with a physician on site). In ketamine treatment the physician explains the treatment, what to expect, and goes over standard safety items associated with ketamine. Treatment begins much as it does in any typicl physicians office, while the patient sits or reclines, and depending on how it was administered, the entire procedure generally takes anywhere from 20 to 40 minutes, after which time you are required to remain at the office for another 90 to 120 minutes so that you can be monitored, until such time you are considered safe to leave. You are not however, permitted to drive and it is suggested that you do not operate heavy machinery, and preferably have planned to take the day off. It is suggested that you arrive home with a therapy appointment in hand, scheduled that day or as soon as possible thereafter while you are still under some level of the drug still in your system, the closer in time between the two, the better.
In psychedelic parlance, we refer to set and setting, emphasizing the importance of these other factors in influencing the overall experience, and not just the effect of the drug itself. Set refers to the mindset of the individual, taking into account psychological stability and mental health issues, current mood, personality, and factors attributable to the inner self. Setting refers to the external world, the physical environment where the experience takes place. Setting includes the feel of the location, building or room, interior design if indoors, the presence or absence of other people including animals, familiarity with the location and people, and cultural sensitivities and social attitude and judgment of those present.
While ketamine treatment and KAP are each concerned with set, KAP also emphasizes setting, and in this case, setting includes the placement in time of the therapy. Typically, KAP is conducted in a room that more resembles a spa than a medical office. The room should be low lighting (but never lights-off as darkness increases the intensity of the dissociative experience), soft, transcendental-oriented, new-wave-ish music, and, barring any complication, only two persons other then the recipient, the physician and the therapist should be present. The treatment room is not appropriate for trainees, graduate students, or interns for several reasons, one of which closely speaks to setting, the other pertaining to HIPAA privacy, in KAP, it is considered a therapy session.
The role of the therapist is crucial to all forms of ketamine treatment, but particularly for KAP and for two reasons. First, having a trusted therapist present and in close proximity, increases the feeling of emotional safety and openness to the dissociative experience. The other role of the therapist is arguably the more important; this is the person who will be talking to you about the issues that brought you to therapy in the first place and the reason you are receiving ketamine, and it begins the moment the ketamine hits your system. Following any initial instructions from the physician, or intervening issues, the therapist will guide you through the experience. The communication that occurs during the dissociative episode is crucial to your recovery. That said, the following section discusses the value placed (how much and if any) of the dissociative experience.
By definition, a dissociated state is a state of mind that includes a strong uncomfortable detached feeling of separation between your physical body and your mind, where you are disconnected to and disoriented from time and place, feeling detached from memories and self. The feeling is usually one of floating above, watching and seeing without judging, being hyper present and feeling adrift simultaneously. The pathophysiology of dissociation should help explain ketamine's efficacy. It has been asked if meditation is the same or a similar experience to dissociation, with or without ketamine. The answer is, unless one is acutely dissociating within the meditation " categorically No". Meditation is powered by the meditator, and the act of conscious letting go implies control of one's thoughts, and actions. In a dissociative state, you are neither relaxed nor in control. Suffice it to say, not being in control is not synonymous with being out of control.
Dissociation
The fifth edition of The Statistical Manual of Mental Disorders (DSM-5) defines dissociation as a disruption of and/or discontinuity in the normal, subjective integration of one or more aspects of psychological functioning, including - but not limited to - memory, identity, consciousness, perception, and motor control. The neural underpinnings of dissociation remain as unclear and cloudy as the felt experience itself. Research suggests that dissociation is likely associated with alterations in brain connectivity and neural networks. Functional neuroimaging results demonstrate changes in brain regions involved in emotion regulation, memory processing, and self-awareness during a dissociative episode. There is also evidence linking to dysregulation of the autonomic nervous system (ANS) which controls physiological responses to stress and emotional states. Individuals with a dissociative disorder tend to show abnormal ANS responses such as increased heart rate, blood pressure and altered skin conductance.
I vividly recall the world events that culminated in 1990 when Brian Keenan, an Irish citizen teaching at American University in Beirut at the time when he was snatched clean off the sidewalk enroute to his classes, where he would spend every minute for the the next four and a half years, gagged, blindfolded, beaten at times near death, starved, and otherwise driven insane, spending as much as four-months at a time in solitary confinement in a filthy moldy underground tunnel fed with with exact same bread meal day after day after day. Only toward the end of his capture was he placed with the other seven hostages. Upon his release from what was infamously called the Iranian Hostage Crisis, Brian wrote extensively about his experiences, much of which he spent in an extended dissociative state from hell. I keep a copy of it in my office...
Hostage is a crucifying aloneness. It is a man hanging by his fingernails over the edge of chaos, feeling his fingers slowly straightening. Hostage is the humiliating stripping away of every sense and fibre of body and mind and spirit that make us what we are. Hostage is a mutant creation filled with fear, self-loathing, guilt, and death-wishing. But he is a man, a rare, unique and beautiful creation of which these things are no part (Keenan, 1990).
Psychological Trauma and Dissociation
The brain and the mind are not always as in sync as one might think. The brain is, in total, a rather physically unappealing 3.5 pounds of gelatinous goo that includes the cerebrum, the cerebellum, the brainstem, and the limbic system. It receives direction by way of chemical or electrical messenger. It does not think. It neither ponders nor questions, and under normal, non-traumatic circumstance, it certainly does not decide. It takes orders and occasionally fulfills requests. With an exception. Your brain will never allow you to take your own life, unless there is considerable damage, temporarily or otherwise, to the neural networks associated with the prefrontal cortex (PFC), the amygdala, the hippocampus, and the serotonergic system, the very regions of the brain implicated in depresssion, suicidal ideation, PTSD, and high anxiety. The brain operates strictly on a system of pattern recognition. It neither knows nor cares if the pattern it detects is healthy or unhealthy, good or bad. Simply If this, then that.
The mind on the other hand, is generally synonymous with the executive functions that cytoarchitecturally speaking, reside within the prefrontal cortex. and represent a conceptual collection of thoughts, perceptions, beliefs, opinions, mental processes, reasoning, judgment, decision-making, impulsiveness, emotions, and all of the thinking, feeling aspects of who we are, including our personality and identity. The mind thinks and processes. The brain more or less takes orders, rarely acting on its own unless there is a disturbance that happens to conflict with your staying alive.
When given a new medication or taking a substance that the brain does not recognize, it assumes you are about to die, and takes coercive measures forcing you to rid yourself of the offending substance. This is the process behind side-effects from a new medication and withdrawal sans titration. You take the pill. The brain is immediately alerted to a foreign enemy. It causes you pain and discomfort, you continue to take it overriding the wishes of your brain, and all things equal, within a few days side effects are no more. Your brain has just registered the event as something that it can now detect. Ten days later you stop the medication cold and in recognizing the error of way, the beast has emerged ready to rescue you yet again. Your brain detected the pill as an enemy but as you continued taking it, the brain was assured that you are no longer in danger and has added the pill event as a detectable substance. But when you stopped taking the pill, you enraged the beast again, and again in a few hours, days or weeks, it will record over the previous event rending the the pill as no longer a recognizable thing. You see the problem?
When a traumatic even occurs, either a single powerful event or one that is ongoing, the brain reverberates with horror as if it has been physically struck. Have you ever looked at a smiling, otherwise calm baby or infant when a loud noise is suddenly introduced? There is the briefest moment of stunned silence followed by an ear-piercing wail. The human brain is not hardwired to deal with a psychologically traumatic event. Not unlike what you might encounter if lightening or a tsunami hit your computer, leaving you with a mass of tangled, half dangling, half fried unrecognizable wire. The intensity or continuous damage to the wires, will determine whether or not your computer will operate in part or at all, and the parts that might miraculously work, may not be in the best working order. Same with the brain, with one extraordinary difference...
When the human brain experiences a traumatic event, it immediately conserves energy and reduces output to those systems essential to survival. This is shock, and it appears to yourself and others, that you are suddenly in a world going slo-mo. Shock is in fact dissociation. You are instantly cut off from the normal realm of experience as if you are somehow floating above the earth, disconnected from the present. Regardless of injury, pain and fear are no longer experienced to the conscious self. The problem going forward, every time you experience an emotion that the brain detects as identical or similar enough to the emotional experience from the traumatic event, like that little pill, it once again comes to the rescue, and floods your brain and body with a cascade of noxious cortisol, that in large doses, will be, under this scenario, responsible for the dissociative episodes experienced throughout the lifespan unless or until you receive trauma treatment to reset your brain.
An important note...Since the brain has made the traumatic event and the concomitant emotional fallout as part and parcel of the normal experience of being you, if you are fortunate enough to go through life for a period of time without a major psychological event, the brain will once again come to your rescue under the assumption that trauma is the new normal, and your brain, dysregulated from the impact of a traumatic event, will coerce you to seek out danger, arousal, negative excitement, or most likely, a manufactured facsimile of your original trauma. . Famed director Alejandro Jodorowsky, is known for saying, among other things,
a bird born in captivity thinks flying is an illness.
The brain does as it does and knows what it knows, and everything else is a mortal enemy.
The question concerning the potential danger of a drug-induced dissociative episode appears answered, in part... imagine for a moment if, within 24-hours of a traumatic impact, your trauma-informed psychotherapist were there with you, taking you through the experience while your brain and your mind are open and at its most vulnerable, without changing one iota of the actual narrative... the sights and sounds and smells and texture of that horrific event, in essence the sum total of that devastating experience would remain as a memory but without the horror attached to it. Your brain, under that dissociative episode while it is open and absent fear, the neural underpinnings , the traumatic experience at a molecular level, has been desensitized. The damage to your brain and your mind would be reset. The incident remains, but you are no longer triggered by it. It has become a part of your story with no particular intensity or emotionality attached to it. This is discussed further in my next blog posting on the psychedelic brain.
Psychotherapy and the Ketamine Connection
Serious and lasting change does not occur in a vacuum, and neither does Ketamine therapy, and for similar same reasons. The therapeutic relationship is a vital component of the therapeutic process and in and of itself, produces important changes in the brain essential to healing, a particularly crucial factor for those impacted from early childhood maltreatment. While healing from a surgical procedure requires trust in the physicians surgical ability and little else, emotional healing, especially from core wounds, such as a betrayal trauma, requires trust in the process and the person guiding that process, in order to reset that part of your brain that was psychologically impacted.
The therapeutic relationship enables the brain to course-correct for the betrayal experienced in a prime relationship. While evidence-based methods appropriate to the person and the diagnosis help move the process along, delivering evidence-based tools to help you navigate the terrain, care remains unconditional and boundaries inviolate, further enabling the individual to open up, speak freely, and receive the help offered without fear..
Psychological trauma in general, but betrayal trauma in particular triggers the release of a copious amounts of cortisol from a neuroendocrine system known as the hypothalamus-pituitary-adrenal axis (HPA). Chronic activation of this system and the ensuing cascade of free flowing cortisol is responsible for significant damage to a host of bodily, neurological functions and is often the culprit in a variety of psychiatric disorders.
Plucked from ancient Greek literature, parrhesia refers to the ability to speak truth to power, to speak freely to authority, without consequence; to open one's heart and mind to another. Psychological trauma prevents or at the very least impinges on the ability to trust and without trust to express ones self freely. The opposite side of the same coin is the construct of alexithymia, also borrowed from the Greek, referring to a damaged neurological state that results in the inability to recognize or verbalize one's own emotional state. Only slightly less horrifying than looking in the mirror and not recognizing who is staring back at you, Alexithymia is part and parcel of the PTSD symptom picture.
It has been suggested that Alexithymia occurs as a result of disruption to areas of the anterior cingulate, the amygdala, and the prefrontal cortex (PFC); all areas with an abundance of NMDA glutamate receptors that ketamine has a known affinity for, inhibiting the otherwise typical excitatory effects of glutamate.
PTSD and C-PTSD and the Ketamine Connection
Severe trauma forces a person to float in a disorienting sea of malevolence and uncontrollability,
leaving the traumatized brain with what becomes the classic adaptation to life; awash in a hostile and unpredictable environment, and left with profoundly impaired attachments and unmetabolized rage. It dismantles the very core of our assumptive world views. Daniel Alkon reminds us that …memory’s permanence maintain’s trauma’s grip on our behavior, leaving the impacted brain stuck in a vicious loop of trying to maintain relatively high levels of cortical stimulation resulting in impulsive, self-injurious and erratic behaviors, while simultaneously spending considerable time and energy in an ongoing battle of emotional arousal-arousal reduction.
A traumatic event has a profound and immediate impact at the molecular and cellular levels of the brain. At the cellular level, hippocampal neurons, crucial for memory formation, may atrophy, while the amygdala, involved in fear and emotion intensity, increase in both size and activation. At the molecular level trauma impacts serotonergic, dopaminergic, and norepinergic neurotransmitters, each of which play a sizable role in mood and stress regulation, leading to a cascade of hormonal changes, most notably that of cortisol, a major contributor to chronic stress.
We have known for quite some time that trauma highjacks and rewires the brain, and for those with childhood trauma and chronic maltreatment, inescapable trauma alters the trajectory of what would otherwise be a normal course of neural development, into something painfully different that if left untreated, can and often does, create a lifetime of unending confusion, pain, and unmanageability, affecting learning, memory, planning and decision-making, arousal dysregulation and the inability to self-soothe, leaving one bereft of the ability to experience healthy attachments, and live an otherwise meaningful productive life.
Auvelity, the Ketamine Alternative
A promising new antidepressant marketed as a ketamine alternative, is out on the market. On August 19th, 2022, the FDA approved Auvelity (dextromethorphan-bupropion) for use as an antidepressant for the treatment of MDD in adults. If the generic name seems oddly familiar, you are not alone. There is a good chance you might have a bottle of dextromethorphan (DXM) somewhere in the back of your medicine cabinet; it is a widely-used ingredient in OTC cough medicine working as a cough suppressant, since the 1950s. Of particular interest, at higher doses (7.5 -15 mg/kg, dextromethorphan induces intense hallucinations, dissociative symptoms, and agitation similar to subanesthetic doses of ketamine.
The second ingredient, bupropion, is the generic name for Wellbutrin, one of the most prescribed antidepressants, and up until now, is one of a rare few antidepressants that does not work on serotonin. Bupropion is a highly effective antidepressant as is, so why the addition of a cough syrup molecule? Dextromethorphan, as it turns out, is a non-competitive N-methyl D-aspartate (NMDA) receptor antagonist and sigma-1 receptor agonist, and bupropion is an atypical norepinephrine-dopamine reuptake inhibitor (NDRI).
Auvelity is a first-of-its-kind NMDA receptor antagonist antidepressant, and is touted as a ketamine-like pill for MDD. As we know with ketamine, dextromethorphan acts as an NMDA receptor antagonist thereby increasing glutamate levels as well as serotonin levels. Buproprion also increases the availability of dopamine by blocking its reuptake. The two together increase the availability of norepinephrine by inhibiting its intake. The rationale behind this otherwise innocuous mix is interesting; unfortunately, dextromethorphan is quickly metabolized by the cytochrome CYP2D6 when taken orally, making it nearly impossible to maintain any semblence of a therapeutic dose. But, when bupropion is added to dextromethorphan, the same cytochrome (CYP2D6) that causes dextromethorphan to be quickly metabolized, is inhibited by the addition ofBupropion.
What distinguishes Auvelity from all other antidepressants, mah nishtanah? All other antidepressants require a two at minimum, more likely a three-week window before attaining full therapeutic dose. While the rather astonishing rapidity with which oral Auvelity reaches its full effect is a major draw, a significant drawback, according to some, between Auvelity and ketamine, is the absence of a dissociative induction despite knowing the literature remains mixed on whether the dissociative component of ketamine is necessary for the rapid and full, albeit semi-temporary cessation of depression and suicidality.
Ketamine treatments range anywhere from $350 per treatment to $600 per treatment, while one center in Texas advertises their ketamine treatment starting at $600 for a single treatment or the standard treatment package in excess of $7,000. With the exception of Spravato, I know of no insurance carrier that will pay for off-label ketamine. Until there is a generic version of Auvelity which is not arriving anytime soon, a 30-day supply of 45 mg - 105 mg extended release pills cost $561 per bottle, with a steep discount for those with insurance.
 RSS Feed
RSS Feed